baseline characteristics
The baseline characteristics of the four groups are shown in Table 1. The aggression minimization and minimization groups were older than the other two groups. The most common underlying liver disease in HCC was hepatitis B in all groups, with significant differences. Pre-transplant model end-stage liver disease (MELD) scores were significantly different between the four groups, with minimal differences in median values. The proportion of living donors was >75% in all groups. Donor age, sex, and graft steatosis were similar between groups. The median AFP of the conventional exposure group, active minimization exposure group, minimization exposure group, and high exposure group were 6.5, 8.0, 5.6, and 11.0 ng/mL, respectively (P = 0.009). PIVKA II at LT were 31.5, 113.5, 38.0, and 28.0 mAU/mL (P < 0.001), with significant differences between groups, with higher values in the radical minimization group. The type of bridging therapy differed significantly between groups, with a higher incidence of systemic therapy or radiation therapy in the minimally invasive and minimally invasive groups (11.9%, 37.5%, 17.4%, and 5.9%, respectively; P < 0.001). Regarding explant pathology, most variables were similar between groups except for poor differentiation and satellite nodules. The four groups had similar HCC risk categories according to Milan criteria and French risk score.
Immunosuppressants
In the entire study population, TAC was initiated at least 4 days postoperatively. Nearly all but one patient received induction therapy with an interleukin-2 receptor antibody, with a total dose of 40 mg in 99.0% of patients. Three months after LT, 33.3% of patients were taking MMF and 31.8% were taking mTOR inhibitors (Fig. S1).
The CET group was well stratified by median tacrolimus trough levels throughout the study period (Fig. 2). Parameters related to intrapatient variability showed significant differences between groups. In particular, the coefficient of variation observed in the aggression-minimized group was higher than that of the other groups (Table S1). Immunosuppressive treatment regimens also differed between groups. In the high-exposure group, the proportion of TAC monotherapy was the highest (31.0%, 12.5%, 26.9%, and 68.0%, respectively), and the proportion of TAC+mTORi treatment showed an opposite trend with the degree of CET (22.7%, 81.2%, 48.4%, 2.0, respectively). %). Oral steroid maintenance was similar for most patients in the four groups.
HCC recurrence and overall death
During a mean follow-up period of 43.2 ± 20.2 months, 74 (14.5%) patients developed HCC recurrence and 77 (15.0%) patients died. The median duration from LT to HCC recurrence was 13.4 (IQR 9.4–23.1) months (Fig. S2). Using Kaplan-Meier analysis, there was no significant difference in 5-year recurrence-free survival rates among the four CET groups (84.0%, 74.2%, 84.5%, and 84.2% for the conventional, aggressive minimization, minimization, and high-exposure groups, Respectively, P = 0.671; Figure 3a). In contrast, there was a significant difference in 5-year overall survival between the groups, with the minimal-aggression group and the high-exposure group having lower survival rates than the other groups (85.6%, 70.5%, 85.2%, and 76.2%, respectively , P = 0.004, Figure 3b). The distribution of causes of death is shown in Figure S3, and there was no statistical difference.
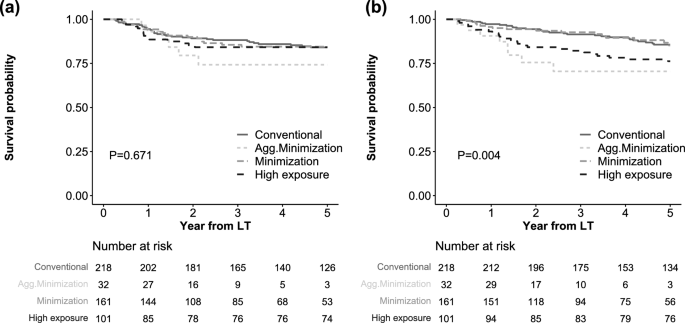
Kaplan-Meier analysis of survival outcomes. (arrive) HCC recurrence = no survival, (Second) overall survival rate.
In univariate and multivariate Cox analyzes (Table 2), the CET group was not a significant risk factor for HCC recurrence (HR for aggressive minimization 1.13, P = 0.790; HR for minimization 0.99, P = 0.973; HR for minimization 0.94, P = 0.848 high exposure vs. traditional exposure). Other important risk factors for HCC recurrence include age (HR 0.95, P = 0.004), BMI (HR 0.92, P = 0.033), pre-transplant MELD score (HR 0.94, P = 0.017), log AFP (HR 1.18, P = 0.017). Bridging therapy (no bridging therapy, HR 0.21, P = 0.001; systemic or radiotherapy versus local therapy, HR 2.38, P = 0.003), number of viable tumors (HR 1.07, P = 0.006), maximum tumor size (HR 1.13, P) = 0.044), microvascular invasion (HR 2.14, P = 0.005), and acute rejection within 3 months (HR 2.10, P = 0.006).
In contrast, in multivariable analysis, aggressive minimization was a significant risk factor for overall death compared with the conventional group (HR 5.19, P = 0.001). Minimization did not affect overall mortality (HR 1.16, P = 0.640), and the high-exposure group showed a marginal risk (HR 1.64, P = 0.091) compared with the conventional group. Other risk factors for death included BMI (HR 0.91, P = 0.012), deceased donor (HR 2.00, P = 0.008), log AFP (HR 1.18, P = 0.007), systemic or radiotherapy versus local therapy (HR 3.71, P < 0.001), number of viable tumors (HR 1.06, P = 0.006), satellite nodules (HR 4.52, P < 0.001), and mTORi use within 3 months (HR 0.25, P < 0.001).
Matched analysis and subgroup analysis of HCC recurrence
We performed a matched analysis of HCC recurrence between the conventional CET group and the other three CET groups. Baseline characteristics were well balanced between matched groups (Tables S2–S4). The results also showed that there was no significant relationship between the CET group and HCC recurrence (Fig. S4). We also performed subgroup analyzes stratified by HCC recurrence risk, such as within/above Milan criteria, French risk score ≤ 2/> 2, with/without systemic therapy or radiotherapy before LT, and with/without mTORi (Fig. 4) . However, no significant differences were observed between CET groups in these subgroups.
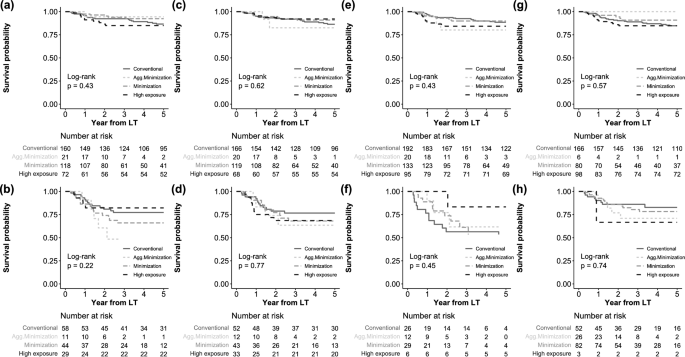
Subgroup analysis of HCC recurrence. (arrive) in Milan, (Second) above Milan, (C) France risk score ≤ 2, (d) France Risk Score > 2, (and) does not require systemic therapy or radiation therapy, (F) undergo systemic therapy or radiation therapy, (G) does not have mTORi, and (H) with mTORi.

