Since the discovery of HIV in the 1980s, the outlook for people with the disease has improved dramatically. With recent advances in antiretroviral (ARV) drugs, including cocktails of drugs that prevent the virus from developing drug resistance, patients who continue treatment after testing positive can now expect to live long, healthy lives, and The risk of later developing AIDS is very low.
challenge: Even so, antiretroviral treatment imposes ongoing costs on patients’ quality of life. To maintain drug levels high enough to suppress HIV in the blood, they need to follow a strict treatment regimen—each drug requires a different dose and frequency of administration.
For many people, the need to constantly keep track of such a complex treatment plan is stressful and difficult and provides a constant reminder of their condition.
Hydrogels: New research published in Journal of the American Chemical Society The possibility of a more subtle approach to delivering HIV treatment is described. In their study, Honggang Cui of Johns Hopkins University and colleagues describe how injectable hydrogels can be used to deliver antiretroviral drugs directly into the bloodstream.
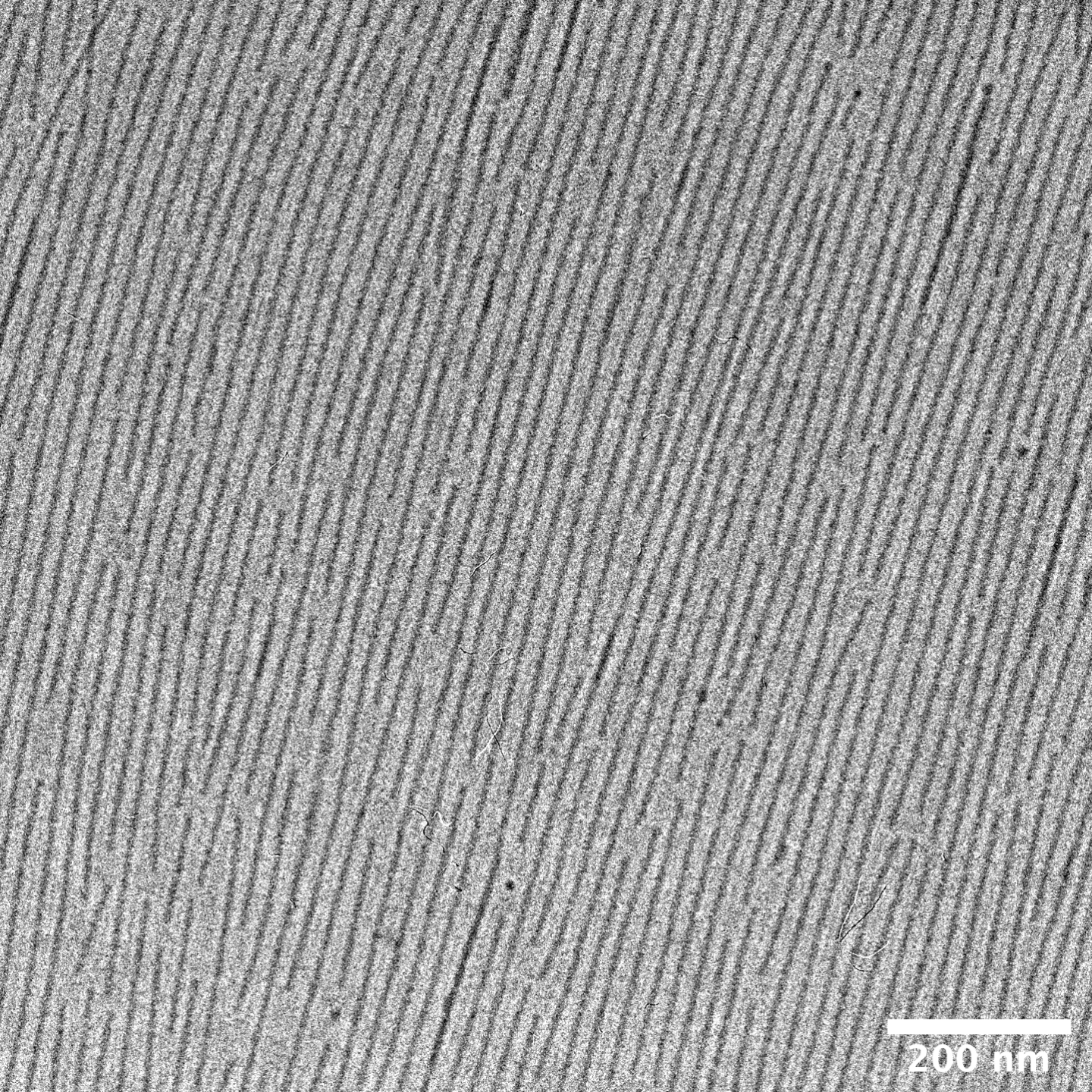
Hydrogels, widely used in medicine due to their similarity to biological tissue, consist of a 3D network of polymer chains that can absorb and retain large amounts of water.
After injection, the material dissolves back into individual molecules of the anti-HIV drug lamivudine.
this experiment: Cui’s team designed a series of special molecules based on lamivudine: a key antiretroviral drug used to inhibit HIV replication. These molecules have a combination of water-absorbent and waterproof regions, and under the right conditions, they spontaneously assemble into 3D hydrogels.
When injected into the bloodstream, the substance gradually dissolves back into individual molecules of lamivudine.
The researchers injected the hydrogel directly under the skin of mice and then monitored the levels of lamivudine in the mice’s blood over the next few weeks. As they expected, the hydrogel dissolved stably and predictably over 42 days, with the mice experiencing few noticeable side effects. During this time, lamivudine remains at high enough levels in the blood to maintain effective antiretroviral therapy.
The road to new treatments: The results are very promising and suggest that hydrogel-based treatments may be safe enough to undergo human trials in the near future.
Going forward, Cui’s team suggests that more advanced hydrogels could be programmed to deliver several different antiretroviral drugs simultaneously: different molecules dissolve at different rates to deliver appropriate doses of different drugs.
If implemented, these hydrogels would only need to be injected every few weeks, so patients wouldn’t need to worry about keeping track of any confusing treatment plans.
Taking this a step further, the researchers suggest that new hydrogels could be developed to treat other diseases, including hepatitis B, which often occurs alongside HIV.
While the trial may be closer than ever, the team’s approach is still a long way from FDA approval as an alternative to traditional and proven ARV therapies. Still, they hope their hydrogel therapy could one day help improve the daily lives of millions of people around the world.
We’d love to hear from you!If you have any comments about this article, or if you have any suggestions for future Freethink stories, please email Tips@freethink.com.

