The interleukin-17 (IL-17) family includes six molecules that respond to infection and are also involved in various physiological and pathological processes.A new paper is on Signal Transduction and Targeted Therapy Review the multifunctional roles of IL-17 in the body.
 study: The role of the IL-17 family in disease: from laboratory to clinic. Image credit: Schira/Shutterstock.com
study: The role of the IL-17 family in disease: from laboratory to clinic. Image credit: Schira/Shutterstock.com
introduce
IL-17 includes IL-17A, IL-17B, IL-17C, IL-17D, IL-17E (IL-25) and IL-17F, all of which have related structures. IL-17A, also known as cytotoxic T lymphocyte-associated antigen 8 (CTLA-8), has been extensively studied.
There are five receiver subunits, which are assembled to form different receiver types. The IL-17 signaling family has multiple receptors and ligands with multiple functions.
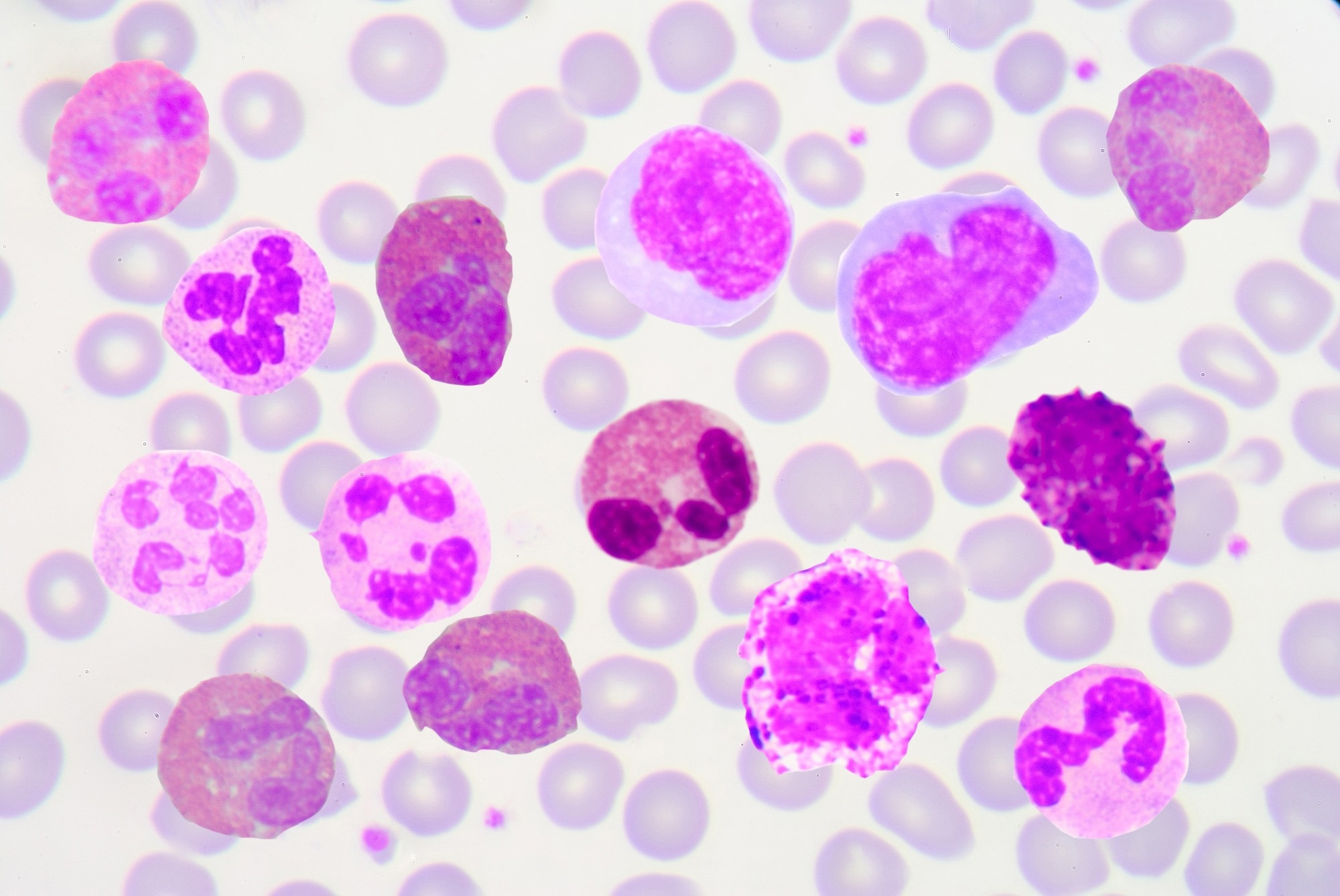
IL-17 is expressed primarily by a subset of CD4+ T helper cells (Th17). IL-17 is also produced by natural killer (NK) cells, CD8+ T cells, dendritic cells, macrophages, and neutrophils during infection.
CD4+ and CD8+ T cells produce IL-17 in response to T cell receptor (TCR) activation. In contrast, innate immune cells produce IL-17 in response to other proinflammatory cytokines, especially IL-1 and IL-23.
IL-17 binds to its receptor IL-17R through the adapter molecule Act1, activating downstream pathways. These involve tumor necrosis factor (TNF) receptor-associated factor (TRAF) and E3 ligase-mediated ribonucleic acid (RNA) binding, inducing transcription and post-transcriptional gene activation.
direct pro-inflammatory effect
IL-17 signaling mediates transcriptional signaling and feedback. IL-17 enhances the inflammatory response by activating the nuclear factor kappa light chain enhancer (NF-κB) and mitogen-activated protein kinase (MAPK) pathways of activated B cells, resulting in the transcription of target messenger RNA (mRNA)). ).
IL-17 is feedback regulated and prevents the inflammatory response from being overly prolonged or overactive.
Another mode of regulation of multiple genes in the IL-17 pathway is through the stability of mRNA transcripts. For example, both the MAPK and NF-κB pathways produce mRNAs with unstable 3′ untranslated regions (UTRs), and RNA-binding proteins (RBPs) such as Act1 can bind to this region, thereby enhancing stability and thus promoting their translation into inflammatory Cytokines. Instead, another RBP called ribonuclease regnase-1 promotes its breakdown.
For IL-17, the unique positive and negative feedback regulatory mechanisms of the signaling pathway make it a mild signaling activator compared with other inflammatory stimuli.“.
In the future, drugs can be developed to antagonize certain autoimmune disease-specific RBPs or to competitively bind to target mRNAs.
synergy
IL-17 works together with other inflammatory signaling molecules, such as interferon gamma (IFNγ), IL-13, and transforming growth factor-β (TGF-β). Conversely, IL-17 pairs with other non-inflammatory cytokines such as epidermal growth factor receptor (EGFR), fibroblast growth factor 2 (FGF2), CARD14 or NOTCH to promote tissue repair, cancer and autoimmune diseases.
CARD14 is elevated in psoriasis and enhances IL-17-induced skin inflammation. Therefore, IL-17 inhibitors may be effective in treating this condition.
Physiological effects
IL-17 increases neutrophil differentiation through the production of granulocyte colony-stimulating factor (G-CSF), monocyte chemoattractant protein-1 (MCP-1), and CXC chemokines by its target cells. Additionally, IL-17 promotes antimicrobial responses, including bronchial-associated lymphoid tissue (BALT) defense against Mycobacterium tuberculosis and immunity against yeast and staphylococcal skin infections.
IL-17 promotes innate immune cells to kill bacteria, prevent mucosal colonization, and enhance cellular defense against intracellular pathogens.
Th17 cells are induced by a variety of viruses, including influenza virus, West Nile virus, and adenovirus. However, human immunodeficiency virus (HIV) selectively depletes memory Th17 cells, thereby reducing their numbers and generating a Th1 response. The disease progresses to immunodeficiency through the development of a dominant regulatory T cell (Treg) profile.
IL-17 stimulates macrophage activity and neutrophil recruitment, primarily protecting against intracellular parasite infection. For example, it also promotes the development of inflammatory granulomas and fibrotic sequelae following liver fluke infection.
IL-17 may exacerbate viral damage, thereby worsening outcomes in viruses such as dengue, hepatitis B (HBV), HCV, and gammaherpesviruses. Thus, IL-17 has both protective and pathogenic roles during certain infections.
In coronavirus disease 2019 (COVID-19), IL-17 has been implicated in the cytokine storm leading to acute respiratory distress syndrome (ARDS) and critical illness.
IL-17 also helps build tight epithelial barriers in the skin and gut, thereby maintaining tight junctions, increasing the production of antimicrobial defense molecules, and activating stem cells to repair damaged areas. IL-17 also promotes bone stability and healing by activating osteoblasts.
Pathological effects of IL-17
Under normal circumstances, IL-17 remains at a stable low level; however, if it is elevated for a long time, it can cause malignant transformation and autoimmune phenomena. IL-17 is elevated in psoriasis, psoriatic arthropathy, and ankylosing spondylitis because it is released by Th17 cells, neutrophils, and CD8+ cells.
IL-17 levels are higher in patients with inflammatory bowel disease. Use of IL-17 blockers was not associated with exacerbation or new onset of these conditions.
IL-17 levels are elevated in systemic lupus erythematosus (SLE) but do not have any direct relationship with severity or symptoms. The true association may be with other Th17 cell cytokines such as IL-21 and IL-22, and possibly indirectly with IL-17. IL-23 promotes Th17 cell differentiation and proliferation, and monoclonal anti-IL-23 antibodies have shown promise in the treatment of active SLE.
Since the Th17/Treg ratio is biased in SLE, restoring the ratio of Treg cells may modulate inflammation and reduce the severity of the disease. Other possible treatments include antagonists that promote IL-17 activation of B cells, monocytes, and plasmacytoid dendritic cells, some of which produce anti-double-stranded DNA antibodies.
Experimental autoimmune encephalomyelitis (EAE) is partially attributed to IL-17 activity. Multiple sclerosis (MS) patients showed an impressive response to secukinumab, an IL-17 antagonist, in a pilot study; however, further studies are needed to confirm this Effect.
The role of IL-17 in cancer
Chronically elevated IL-17 levels in chronic inflammation may increase mutation rates and precancerous cellular changes, thereby making individuals more susceptible to cancer. IL-17 also promotes tumor progression by increasing cell proliferation and metastasis rates as well as immune tolerance of transformed cells. This is supported by the observation of abnormally high IL-17 levels in the tumor microenvironment.
IL-17 may have both pro- and anti-tumor properties in the same type of cancer“.
IL-17 inhibitors in autoimmune diseases
Given the role of IL-17 in many autoimmune diseases (AIDs) such as psoriasis, psoriatic arthropathy, and SLE, monoclonal antibodies (mAbs) against IL-17 have been studied in search of effective treatments . Two approaches have been used, including direct anti-IL-17 antagonists and indirect blockade by inhibiting Th17 cell differentiation.
Some direct anti-IL-17 antagonists including mAbs, such as secukinumab, ixekizumab, and brodalumab, have been approved by the U.S. Food and Drug Administration (FDA) for the treatment of psoriasis. These drugs target IL-17A, all IL-17 cytokines, and IL-17A respectively.
IL-17 in cancer therapy
IL-17 can promote tumor occurrence and progression, as well as tumor regression. Anti-IL-17C blockade may help lung cancer patients by preventing the development of resistance to anti-programmed cell death protein 1 (PD-1) immunotherapy. Other studies have shown encouraging results when using IL-17 as a marker for cancer treatments targeting IL-17-bearing cancer stem cells.
What’s the impact?
IL-17 is a key molecule in multiple physiological and pathological pathways. Currently, there are several monoclonal antibodies that can eliminate this pathway; however, their cost, inconvenience, and immunosuppression are significant drawbacks. Oral small molecule drugs (SMDs) would be preferable because of their shorter duration of action, cost-effectiveness, and ease of administration.
The main consideration when using IL-17 blockers is the need to preserve host immune function. Further research may help provide better treatments for autoimmune and malignant diseases.
Journal reference:
- Huangfu, L., Li, R., Huang, Y., and Wang, S. (2023). The role of the IL-17 family in disease: from laboratory to clinic. Signal Transduction and Targeted Therapy. doi:10.1038/s41392-023-01620-3.
