patient characteristics
Among 791 children, 108 were diagnosed with EBV-HLH and 683 with EBV-IM. The demographic characteristics of the two samples are shown in Table 1 . The proportion of female patients in the HLH group was higher than that in the IM group (ask= 0.011).In terms of symptoms, patients with EBV-HLH were more likely to have hepatomegaly and splenomegaly, whereas patients with EBV-IM were more likely to have eyelid edema, cervical lymphadenopathy, and tonsillitis (all ask< 0.0001).
Comparison of laboratory test results in patients with EBV-HLH and EBV-IM
EBV-HLH and EBV-IM can cause multi-organ damage; therefore, hematological indicators, liver and kidney function parameters, serum cytokines, and lymphocyte subsets were examined. Unlike patients with EBV-IM, patients with EBV-HLH commonly have cytopenias, hypoalbuminemia, and elevated bilirubin, liver enzymes, triglycerides, ferritin, and lactate dehydrogenase (LDH) (Table 2). D-dimer levels in EBV-HLH were significantly higher than those in EBV-IM, whereas fibrinogen levels were much lower. The median EBV-DNA copy number in the plasma of EBV-HLH patients was approximately 90 times higher than that of EBV-IM patients.
Regarding cytokines, IL-6 levels were similar, whereas IL-10 (median concentration: 499.6 pg/mL vs. 19.9 pg/mL, ask< 0.001) and IFN-γ (median concentration: 629.0 pg/mL vs. 8.2 pg/mL, ask< 0.001) levels were significantly higher in EBV-HLH patients (Fig. 1). The proportion of CD8+T cells in the EBV-HLH group was significantly lower than that in the EBV-IM group (44.7% vs. 56.0%, ask< 0.001), whereas total CD3 + T cell counts were comparable (84.2% vs. 85.30%, ask= 0.07).
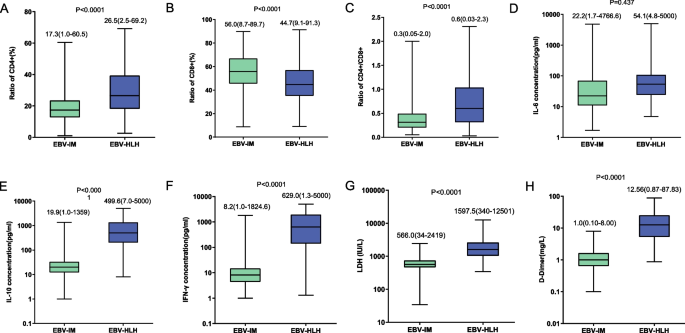
Compare laboratory parameters of EBV-HLH and EBV-IM patients, including the proportion of CD4+ T cells to all T cells (arrive), the proportion of CD8+T cells (Second), CD4 + /CD8 + T cell ratio (C), interleukin (IL)-6 (D), IL-10 levels (and), interferon-γ (IFN-γ) (F), lactate dehydrogenase (LDH) (G) and D-dimer (H)
Since clinical manifestations and laboratory data are affected by patient age, we compared the above parameters in different age groups. Patients were divided into three groups: age ≤3 years, >3 years and ≤6 years, and >6 years. The proportions of CD4+ and CD8+ T cells were different among the three groups, while other parameters were comparable. Comparison results were similar across the three age groups, as shown in the supplementary figure. 1 and 2.
Distinguishing EBV-HLH and EBV-IM through laboratory parameters
Although the severity of EBV-HLH and EBV-IM varies widely, rapid identification and differentiation of EBV-HLH and EBV-IM is challenging due to the lack of early symptoms. Using ROC analysis, we compared the ability of IL-10, IFN-γ, LDH, D-dimer, EBV-DNA copy number, triglycerides, fibrinogen, and ferritin to differentiate EBV-HLH and EBV-IM ( figure 2). The areas under the curve (AUC) for IL-10, IFN-γ, LDH, D-dimer, triglycerides, and ferritin were 0.954, 0.960, 0.895, 0.970, 0.876, and 0.996, respectively, indicating that these indicators have good prediction performance. EBV-HLH. When the cutoff values for IL-10, IFN-γ, LDH, D-dimer, triglycerides, and ferritin were set at 89.6 pg/mL, 45.6 pg/mL, 948.5 IU/L, 3.15 mg/L, 2.1 mmol/L and 429 μg/L, the sensitivities were 87.9%, 90.7%, 81.1%, 91.1%, 81.5% and 98.1% respectively, and the specificities were 98.4%, 96.3%, 89.4%, 94.1%, 80.6% and 96.5%, respectively (Table 3).
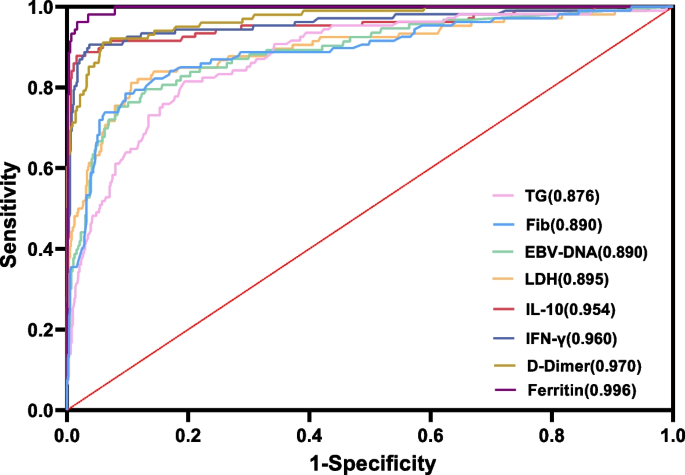
Use triglyceride (TG), fibrinogen (Fib), EBV-DNA serum load, lactate dehydrogenase (LDH), interleukin (IL)-10 (IL-10), interferon-γ (IFN-γ) ROC curve for EBV-HLH prediction), D-dimer and ferritin
Five univariate variables IL-10, IFN-γ, LDH, D-dimer and EBV-DNA copy number, with increasing cutoff values, the positive predictive value (PPV) reached 100% and the negative predictive value (NPV) reduced to approximately 86%. The ideal cutoff value may be the junction of PPV and NPV, which has reference value for clinical differentiation of EBV-HLH and EBV-IM (Figure 3). The maximum cutoff value selected with the intersection point was higher than the value in the Youden index maximum (IL-10: 288.3 pg/mL vs. 89.6 pg/mL, IFN-γ: 240.7 pg/mL vs. 45.6 pg/mL, LDH: 2100 IU/L vs. 948.5 IU/L, D-dimer: 4.50 mg/L vs. 3.15 mg/L, EBV-DNA copy number: 500000 copies/ml vs. 26400 copies/ml), and positive predictive value is also higher (Appendix Table 1).

Positive and negative predictive values of some univariates at different cutoff points. arrive Interleukin (IL)-10 (IL-10); Second interferon-γ (IFN-γ); C Lactate dehydrogenase (LDH); D, D-dimer; E, EBV-DNA loading signal
Predictive model for EBV-HLH
A single variable sometimes fails to differentiate between two entities in earlier stages. Therefore, we developed a prediction model using multiple logistic regression analysis to determine which factors were the most effective predictors. All laboratory indicators with significant differences between the two groups were included, among which IL-10, ferritin, D-dimer, and triglycerides showed statistical significance in multivariate logistic regression analysis. We then developed a logistic regression model based on continuous variables including IL-10, ferritin, D-dimer, and triglycerides (logit ask= -9.969 + 0.057 × IL-10 + 0.006 × ferritin + 0.113 × D-dimer + 0.434 × triglyceride) (Table 4). The AUC of this model was 0.992 (Fig. 4A). The sensitivity and specificity for diagnosing EBV-HLH were 97.96% (95% CI, 92.82-99.75) and 98.16% (96.40-99.20) respectively, and the PPV and NPV were 92.31% (85.79-95.98) and 99.53% ( 95% CI, 98.18–99.88). The positive and negative likelihood ratios were 53.14 (95% CI, 26.73–105.65) and 0.02 (95% CI, 0.01–0.08), respectively. We then used the Hosmer–Lemeshow goodness-of-fit test to evaluate the calibration of the model, which showed that the predictive model had good calibration ability (χ2= 2.077, ask= 0.979) (Fig. 4B).
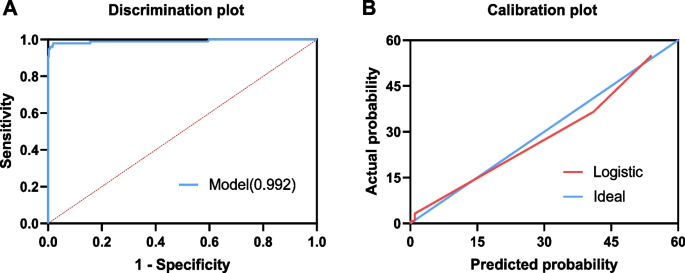
The effectiveness of the model in predicting EBV-HLH was based on a logistic regression model based on IL-10, ferritin, D-dimer and triglycerides. The ROC curve AUC of this model reaches 0.992 (arrive) and plotted the calibration curve of the logistic regression model (Second)
Considering that cytokine assays are not available in some medical centers or that serum cytokine levels may not recover quickly in emergency situations, we established another prediction model based on physical signs and commonly used laboratory indicators. Based on univariate analysis, cervical lymphadenopathy, LDH, D-dimer and triglycerides were included in the logistic regression model, and the AUC of the model was 0.963 (logit ask= -6.187 + 0.002 × LDH + 0.257 × D-dimer + 0.394 × triglyceride -3.049 × cervical lymphadenopathy). The sensitivity and specificity for diagnosing EBV-HLH were 86.32% (95% CI, 77.98–91.83) and 96.53% (94.57–97.79), respectively (Supplementary Figure 3 and Supplementary Table 2).

