Rick Jaenisch underwent six treatments before being cured of hepatitis C in 2017. Each time his doctor recommended a different combination of drugs, his insurance company initially denied the request and then approved it. The process delayed his care for months, even after he developed end-stage liver disease and was awaiting a liver transplant.
“Back then, treatments were supposed to be easily available,” said Jaenisch, 37, director of outreach and education at the Institute for Open Biopharmaceutical Research and Training, a nonprofit organization in Carlsbad, Calif. “He’s an ideal candidate for treatment.”
But it won’t be easy. Jaenisch was diagnosed in 1999, when he was 12 years old, after his father took him to a hospital in San Diego after Jaenisch showed him that his urine was brown, indicating there was blood in it. Doctors determined he was likely infected with the virus at birth. His mother, a dental surgical assistant, learned she had the virus after her son was diagnosed.
This viral disease can be spread through blood, and people who contract it often do well for many years. It is estimated that more than 2 million people in the United States have this type of hepatitis, and 40 percent of them don’t even know they have it, but the virus may be quietly damaging their livers, leading to scarring, liver failure, or liver cancer .
There are now several very effective and low-cost treatments on the market, and it is expected that almost everyone who knows they have hepatitis C will be cured. However, a study published in June by the U.S. Centers for Disease Control and Prevention (CDC) suggests that is not the case. The Biden administration’s proposal to eliminate the disease within five years aims to change that.
Overall, in the decade after new antiviral treatments were introduced, only one-third of people initially diagnosed with hepatitis C cleared the virus, either through treatment or because The virus was removed. Most affected people have some type of health insurance, whether it’s Medicare, Medicaid or private insurance. But even among privately insured patients who were most likely to receive treatment, only half of those over 60 had cleared the virus by the end of the study period in 2022.
“Unlike HIV, which is lifelong, the cure time for hepatitis C is very short, eight to 12 weeks,” said Carl Schmid, executive director of the HIV+ Hepatitis Policy Institute. “So why don’t we do better?”
Experts say those infected face a series of obstacles. Cost is a very important factor when introducing new treatments. Private plans and state Medicaid programs limit spending, make expensive drugs more difficult to obtain, impose prior authorization requirements, limit use to people with already damaged livers, or require patients to forego taking the drugs and use them to qualify, etc.
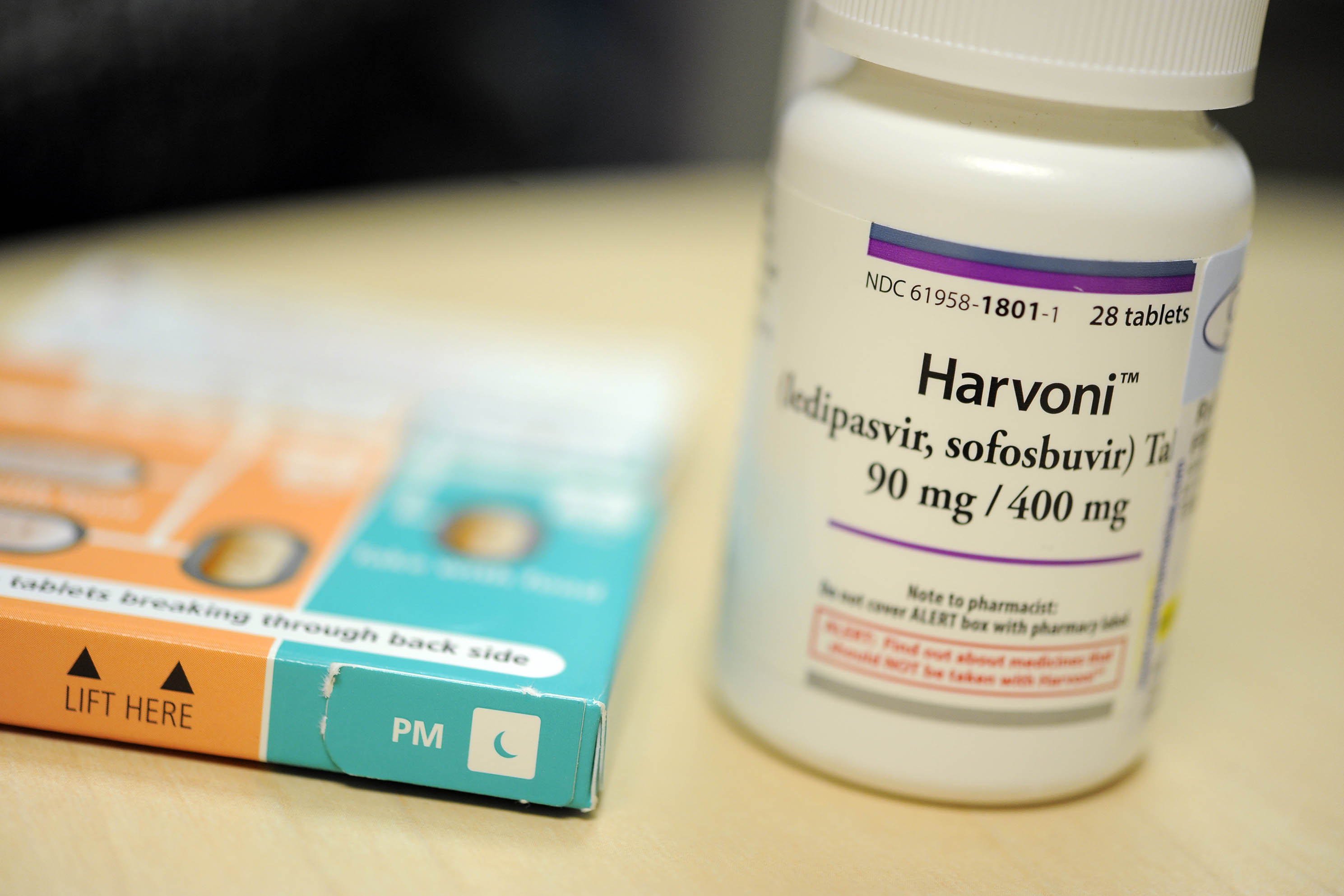
By the time Jaenisch recovered at age 31, the landscape of hepatitis C treatment had fundamentally changed. An innovative once-daily pill was launched in 2013, replacing the grueling regimen of weekly interferon injections, which had uncertain success rates and serious side effects.
The first “direct-acting antiviral drug” treated the disease in 8 to 12 weeks with few side effects and a cure rate of over 95%. As more drugs are approved, the initial price of $84,000 for a course of treatment has gradually dropped to around $20,000.
As drug prices fall, many states have removed some of the barriers that have made it difficult to approve treatments, under pressure from activists and public health experts.
However, there are many more barriers that have nothing to do with drug prices.
Ronni Marks, who lives with hepatitis C, is a voice for patients who are often ignored. These include residents of rural areas and people who are uninsured, transgender or people who inject drugs. An estimated 13% of people in U.S. prisons and detention centers develop chronic hepatitis C infection each year, yet access to care in these settings is limited.
Marks said many vulnerable people need help accessing services. “In many cases, they don’t have the means to travel, or their circumstances don’t allow them to get tested,” he explained.
Unlike the federal Ryan White HIV/AIDS program, which for more than 30 years has provided grants to cities, states and community groups to provide drugs, treatment and follow-up care to people living with HIV, there is no coordinated, comprehensive program for hepatitis C patient.
“In a perfect world, this would be a great model to replicate,” said Sonia Canzater, program director of the Infectious Disease Initiative at the O’Neill Institute for National and Global Health Law in Georgetown. “That may never happen. What we want more than anything is this national program that systematically provides access so that people are not locked into the policies of their state.
The national plan Kanzate was referring to is a $12.3 billion, five-year plan to eliminate hepatitis C that is included in President Joe Biden’s fiscal 2024 budget proposal. Francis Collins, the former director of the National Institutes of Health, is leading the effort in the Biden administration.
This is what the program does:
— Approval of point-of-care diagnostic tests will be expedited, allowing patients to be screened and begin treatment in one visit, rather than the current multi-step process.
– Subscription models will be used to improve access to medications for vulnerable populations, such as those who are uninsured, incarcerated, on Medicaid or members of American Indians and Alaska Natives. This approach, known as the Netflix model, allows the government to negotiate a flat rate with drug companies to cover the cost of treatment for all individuals in a group in need.
— Public health infrastructure will be built to educate, identify and treat people with hepatitis C, including supporting universal screening; expanding testing, provider training and additional support for care coordination; and connecting people to services.
Collins pointed to an analysis by Harvard University researchers that said the plan would prevent 24,000 deaths and save $18.1 billion in health care spending over 10 years.
Collins noted that legislation to implement Biden’s plan, currently in the draft stage, is expected to be introduced when Congress reconvenes after its summer recess. The Congressional Budget Office has not yet estimated its cost.
Before the Covid-19 outbreak in 2020, hepatitis C killed more Americans each year (nearly 20,000) than any other infectious disease. Activists are pleased that the virus is finally getting the attention they feel it deserves. Even so, they don’t believe Congress will support more than $5 billion in new funding. The remainder will be provided in the form of savings from existing plans. However, they believe it is a step in the right direction.
“I’m excited” there’s a federal proposal to end hepatitis C, said Lorren Sandt, executive director of Ambassadors of Care, a nonprofit in Oregon City, Ore., that helps people manage chronic diseases like hepatitis C. disease. “I’ve cried so many times since it’s been made public that I’ve been happy.”