The Hanyang University Hospital Institutional Review Board approved this study without requiring informed consent due to its retrospective nature (IRB No. HYUH 2021-09-013). All methods were performed in accordance with relevant guidelines and regulations.
study population
We reviewed consecutive patients who underwent MRI-PDFF between January 2015 and January 2021. They were referred to tertiary referral hospitals for further evaluation of liver disease of various etiologies. Among them, we included patients who underwent B-USG within 6 months of the MRI-PDFF examination date. We then excluded patients who: (1) were unable to perform B-USG or the interval between B-USG and the date of MR examination was more than 6 months, and (2) were technically unable to measure the mean PDFF value of MRI-PDFF (Fig. 1).

Flow diagram of the study population. B-USG B-mode ultrasound examination, chronic liver disease chronic liver disease, FL fatty liver, LC cirrhosis of the liver, Magnetic Resonance Imaging PDFF Magnetic resonance imaging proton density fat fraction.
B-ultrasound examination
Three abdominal radiologists with 10, 6, and 4 years of experience in abdominal imaging used four different B-USG scanners (EPIQ 5Q or IU-22, Philips Health Care, Best, The Netherlands; Aixplorer, SuperSonic Imaging, Aixen-Provence, France; RS85, Samsung Madison, Seoul, South Korea). They evaluated FL disease and qualitatively divided FL into the following three stages: (1) mild: mildly increased liver echogenicity compared with renal echogenicity; (2) moderate: enhanced liver echogenicity compared with renal echogenicity, The vision of the liver blood vessel wall and diaphragm is slightly impaired; (3) Severe: Compared with the kidney echo, the liver echo is significantly increased, the posterior shadow, and the liver blood vessel wall and diaphragm are not visible.In cases of chronic kidney disease or absence of the right kidney, where it is difficult to compare liver echo intensities, we can also use spleen echo intensities13,14 (figure 2). We then retrospectively collected FL diagnostic data based on B-USG reports. CLD or LC were assessed based on B-USG results (eg, liver echogenic roughness or surface nodules) and clinical findings (eg, Fibroscan™ or FIB-4 results).
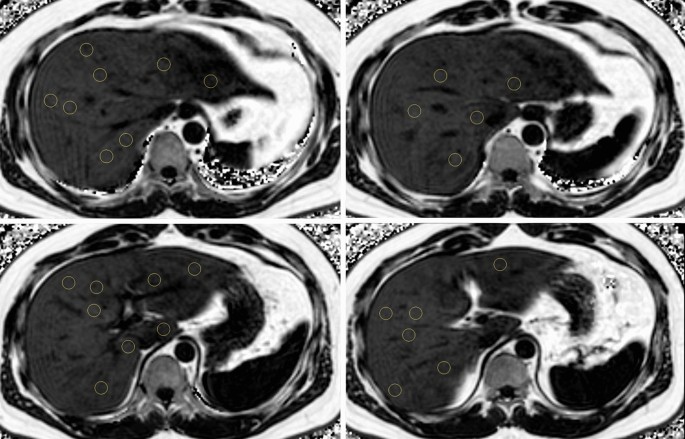
Demonstration image of Magnetic Resonance Imaging-Proton Density Fat Fraction (MRI-PDFF) measurement. Three circular regions of interest (100 mm2 Draw areas within each liver segment) to avoid large vessels, bile ducts, capsules, and space-occupying lesions. The average of 24 measurements per liver segment was considered as the mean MRI-PDFF value.
MRI-PDFF examination and measurement
MRI-PDFF examinations were performed using a 3T MRI scanner (Ingenia or Achieva, Philips Healthcare, Best, The Netherlands) with a torso coil. Three-dimensional multiple gradient echo (GRE) sequences were performed in one breath hold. The parameters of MRI-PDFF are as follows: six echo times (TE) (first TE, 0.98 ms; delta TE, 0.8 ms) and repetition time (TR), 6.3 ms; flip angle, 3°; parallel imaging SENSE factor , 2; signal average, 1; matrix size, 300 × 300; field of view, 350 × 350 mm; number of slices, 60; and 3 mm slice thickness (50% interpolation). We used six echo acquisitions and seven peak fat models to overcome T2* bias and fat complexity. Acquired MRI data were processed using software (ISP; Philips Health care, Best, Netherlands). MRI-PDFF plots were adjusted for confounding variables and generated for the purpose of MRI-PDFF measurements. Then, three circular regions of interest (100 mm2 Draw areas within each liver segment) to avoid large vessels, bile ducts, capsules, and space-occupying lesions. The average of 24 measurements per liver segment was considered as the average MRI-PDFF value, and the right MRI-PDFF value was calculated as the average of 12 measurements in the right hemi-liver. MRI-PDFF measurements were performed by two abdominal radiologists (KMM, KBK) with more than six years of experience in abdominal imaging, and we collected MRI-PDFF measurement data retrospectively based on MRI reports. Based on a previous study, we used a 6.4% cutoff for the presence of FL (mean MRI-PDFF value ≥ 6.4%)fifteen. We also measured abdominal wall thickness, defined as the distance between the liver capsule and the skin at the midaxillary line on axial T2-weighted images, in 206 patients in this study.
clinical parameters
All patients underwent laboratory tests after midnight fasting, and the following laboratory data were obtained: aspartate aminotransferase (AST), alanine transferase (ALT), triglycerides, gamma-glutamyl transferase (GGT) ), high-density lipoprotein (HDL), low-density lipoprotein (LDL), and cholesterol. In addition, we obtained each patient’s age, sex, and body mass index (BMI) through electronic medical record review and calculated BMI using the following formula: BMI (kg/m2) = weight (kg)/(height (m))2.
Inconsistency analysis between B-USG and MRI-PDFF
We created a FL diagnostic confusion matrix between B-USG and MRI-PDFF to classify concordant and discordant results between B-USG and MRI-PDFF. Ultrasound fatty liver (“UFL”) is defined when mild or severe FL occurs on B-USG. FL on MRI (“MFL”) was defined when the mean MRI-PDFF value was 6.4% or higher. Patients were further classified according to the presence of CLD or LC. We identified four discordant groups as follows: (1) “UFL-MnFL-wo” group (B-USG FL–MRI-PDFF no FL, no CLD or LC), (2) “UFL-MnFL-w” group (B-USG FL–MRI-PDFF no FL with CLD or LC), (3) “UnFL-MFL-wo” group (B-USG no FL–MRI-PDFF FL without CLD or LC), and (4) “ UnFL-MFL-wo” group-w” group (B-USG without FL–MRI-PDFF FL with CLD or LC) (Fig. 3).
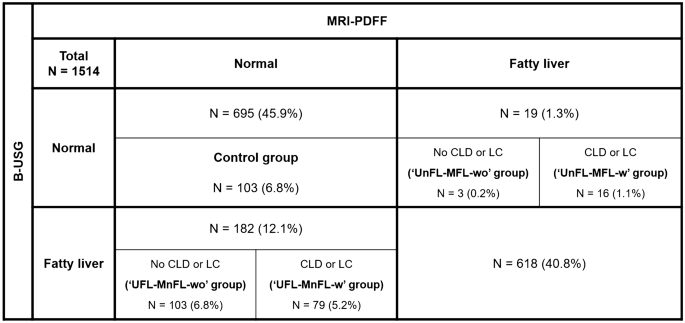
Fatty liver assessment was inconsistent between B-USG and MRI-PDFF. B-USG B-mode ultrasound examination, chronic liver disease chronic liver disease, LC cirrhosis of the liver, Magnetic Resonance Imaging PDFF Magnetic resonance imaging proton density fat fraction.
We also included 103 patients with normal B-USG and MRI-PDFF results (i.e., no FL on B-USG and mean PDFF less than 6.4%) and no CLD or LC for comparison. Compared with the “UFL-MnFL-wo” group, we defined them as the “control group”. The MRI-PDFF values of both groups were within the normal range (less than 6.4%); however, B-USG showed different FL diagnosis results in each group (no FL in the control group, and FL in the “UFL-MnFL-wo” group).
Statistical Analysis
Inconsistency analysis yielded the exact frequency for each inconsistency group. We compared the “UFL-MnFL-wo” group with the control group on various imaging and clinical parameters that may contribute to the differences between the two groups. Continuous variables were compared using independent t tests and categorical variables were compared using chi-square tests. We use MRI-PDFF as the reference standard for FL diagnosis instead of liver biopsy. We used the area under the receiver operating characteristic curve (AUC), sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) according to the presence of CLD or LC.Statistical significance was set to p< 0.05. All statistical analyzes were performed using SPSS version 26.0 (IBM, Armonk, NY, USA).
ethical approval
The Institutional Review Board of Hanyang University Hospital approved this study.

