General patient characteristics
This study included 118 HBV-ACLF patients. Of these patients, 104 (88.1%) were male. The mean age was 41.3 ± 10.7 years. The average HBV DNA level was 3.2 ± 2.2 log10 SI units/ml. The mean model values for end-stage liver disease (MELD) score and MELD-sodium (MELD-Na) score were 27.4 ± 6.8 and 30.4 ± 9.4, respectively. Potential precipitating events included discontinuation of nucleos
All patients were followed for up to 90 days after enrollment. The mortality rate of free transplantation was 39.0%, and the incidence rates of new renal insufficiency, hepatic encephalopathy, and nosocomial infection were 32.4%, 25.7%, and 68.8%, respectively (Table 2). Nosocomial infections mainly include SBP, respiratory infections and other types of infections. See Appendix Table 1 for details. Other types of infections in this study refer to infections outside the abdomen and lungs, involving the urinary and gastrointestinal systems, and unlocalized infections.
Correlation of ESI with baseline characteristics
According to the median ESI (12.05 cm2/rice2), patients were divided into two groups to evaluate factors related to erector spinae muscle mass in patients with HBV-ACLF. The ESI cutoff value calculated by ROC is 12.06 cm2/rice2, very close to the median. Comparison of baseline characteristics between the two groups is shown in Table 1. Patients with ESI<12.05 cm2/rice2 (n = 58) had higher serum ammonia levels than patients with ESI ≥ 12.05 cm (P = 0.030)2/rice2 (n = 60). There were no significant differences in age, MELD score, MELD-Na score, or other laboratory parameters. Further binary logistic regression analysis was used to identify factors independently associated with ESI (Table 3). Presence of hepatic encephalopathy (odds ratio (OR) = 2.26, 95% confidence interval (CI): 2.05–3.18; P = 0.006), SBP (OR = 3.95, 95% CI: 1.01–5.46; P = 0.037) and renal Functional impairment (OR = 4.47, 95% CI: 1.02-9.64; P = 0.032) was independently associated with low ESI in HBV-ACLF patients.
Effect of ESI on free graft mortality in HBV-ACLF patients
During the 90-day follow-up period, 30 of 58 (51.7%) low-ESI patients died and 16 of 60 (26.7%) high-ESI patients died (P = 0.005) (Table 2). Kaplan-Meier survival analysis was performed, and the cumulative survival rates were 71.0% ± 4.6 and 85.8% ± 3.9 (log-rank P = 0.003) (Fig. 2A). The hazard ratio (HR) calculated using univariate analysis was 2.23 (95% CI: 1.25–4.21; P = 0.005), and further multivariate analysis showed that low ESI was associated with an increased risk of death (adjusted HR = 2.52; 95% CI: 1.34–9.24; P = 0.011) (Table 4). Supplementary Tables 2 and 1 provide details of comparisons and multiple analyses, respectively, between surviving and non-surviving patients.
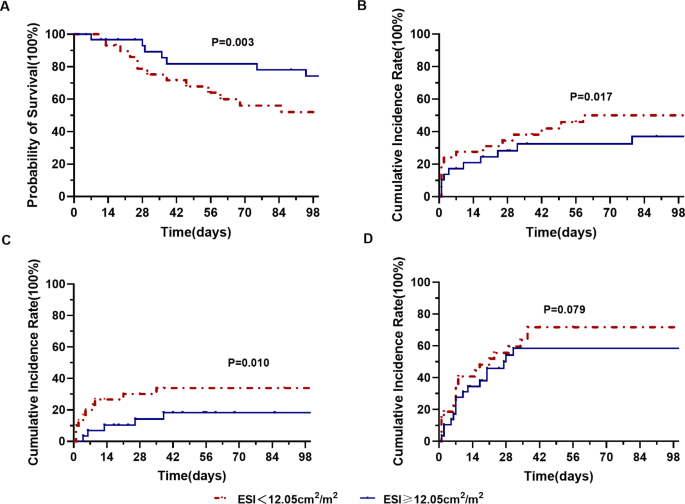
Kaplan-Meier curves for patients with low and high ESI levels.Calculation of statistical significance by log-rank test (arrive) Cumulative survival rate, (two) Cumulative incidence of renal insufficiency, (C) Cumulative incidence of hepatic encephalopathy, and (Four) Cumulative incidence of nosocomial infection
Effects of ESI on renal insufficiency, hepatic encephalopathy and nosocomial infection
In this study, 102 patients had no renal dysfunction at baseline. Among these patients, 20 of 46 (43.5%) low-ESI patients and 13 of 56 (23.2%) high-ESI renal patients developed functional impairment during the 90-day follow-up period (P = 0.029) (Table 2 ). There was a significant difference in the cumulative incidence of renal insufficiency between groups (log-rank P = 0.017) (Fig. 2B). Univariate and multivariate analyzes are shown in Table 4 , indicating that low ESI is an independent risk factor for renal dysfunction (adjusted HR = 1.36; 95% CI: 1.05, 2.93; P = 0.043) (Table 4 and Supplementary Table 4 details ).
In addition, Kaplan-Meier analysis showed that among 105 patients without hepatic encephalopathy at baseline, the cumulative incidence of hepatic encephalopathy was higher in 49 patients with low ESI than in 56 patients with high ESI (39.6% vs 14.0%). %, P = 0.003; log-rank P = 0.010) (Table 2; Figure 2C). By multivariate analysis, low ESI was an independent risk factor for the development of hepatic encephalopathy (adjusted HR = 2.26; 95%) CI :2.05, 3.13; P = 0.036) (Table 4 and Supplementary Table 5 for details). However, there was no difference in the cumulative incidence of nosocomial infection between the two groups (75.0% vs. 63.4%, P = 0.273; log-rank P = 0.079; adjusted HR = 1.62; 95% CI: 0.60, 3.08; P = 0.138) (Figure 2D; Table 4 and Supplementary Table 6 for details).
Correlation between ESI and SMI
Twenty-three patients in this study had whole-abdominal CT images. ESI and SMI at L3 were calculated for these patients. The mean ESI and SMI were 11.7 ± 3.8 and 39.4 ± 12.3, respectively (P = 0.231). There was a significant positive correlation between ESI and SMI (r=0.714, P<0.001). We also evaluated the predictive ability of ESI and SMI for mortality outcomes. The ROC areas of ESI and SMI are 0.755 (0.536-0.973) and 0.773 (0.563-0.983) respectively (Figure 3). ROC analysis did not yield significant results (Z=-1.449, P=0.147).
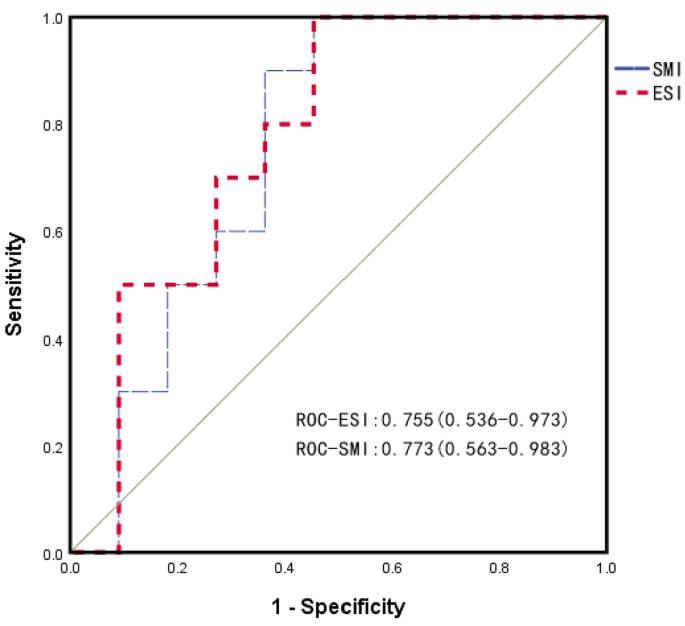
ROC was used to evaluate mortality in HBV-ACLF patients. The area under the ROC (95% CI) for ESI and SMI was 0.755 (0.536–0.973) and 0.773 (0.563–0.983), respectively. ESI: erector spinae index. SMI: skeletal muscle index

